Abstract
Introduction
Warfarin is used in the treatment and prevention of thromboembolic disorders, with the risk of bleeding ranging from 1% to 3% per year resulting in hospitalisation or death. Emergency reversal of warfarin is indicated when warfarin therapy is complicated by bleeding, prior to emergency procedures / surgeries, and in patients who have supra-therapeutic INR with high risk of bleeding. Launceston General Hospital is a 330-bed hospital in regional Australia and we practise warfarin reversal in accordance with the national guidelines. Prothrombinex-VF (PTx-VF) is a 3-factor prothrombin complex concentrate (PCC) used in Australia, which contains factors II, IX, and X mainly. Due to low factor VII levels in PTx-VF, addition of 1 unit of FFP with PTx-VF is generally recommended, however there is lack of supportive evidence. There are a few reports of successful use of 3-factor PCC without the use of FFP. Hence in our hospital, the addition of FFP to PTx-VF for warfarin reversal is based on clinician's preference.
Aim of study
To study the clinical, laboratory, therapeutic and outcome data on patients who underwent emergency reversal of warfarin anticoagulation, and to compare the warfarin reversal (INR values) after administration of PTx-VF vs PTx-VF + FFP.
Methods
We performed a retrospective study of patients who underwent emergency reversal of warfarin in our hospital between January 2011 and December 2013. All the patients who underwent emergency reversal of warfarin with PTx-VF +/- FFP were captured from the blood bank database. Patients who received PTx-VF for indications other than emergency warfarin reversal and those with insufficient data were excluded from the study. The clinical, laboratory and transfusion data of these patients and the warfarin reversal strategies and clinical outcomes across different clinical settings were analysed. Non-parametric statistical analysis was used to compare the differences in post-treatment INR values in the PTx-VF vs PTx-VF + FFP groups and statistical significance was assumed at a P value of less than 0.05.
Results
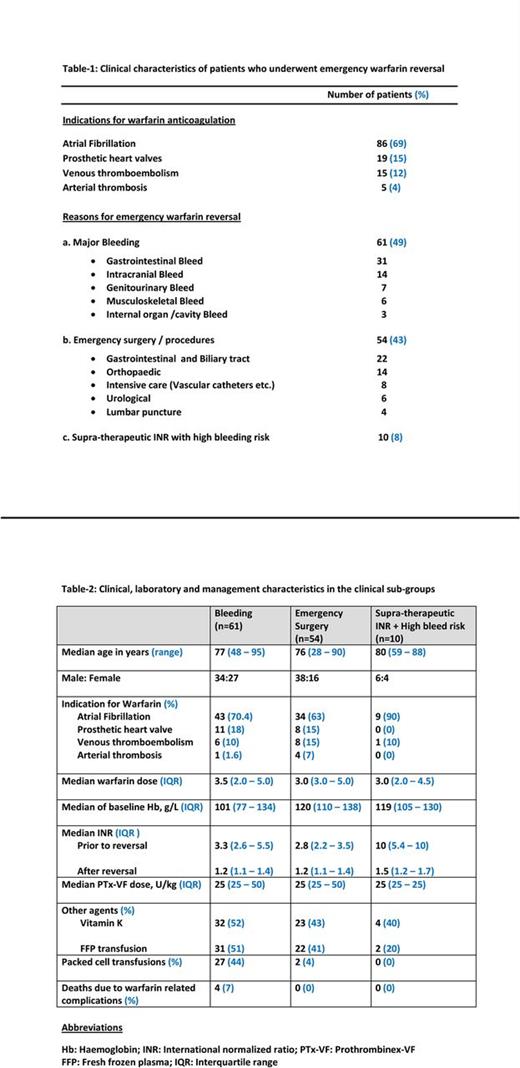
A total number of 125 patients who underwent emergency warfarin reversal were included in the study. The median age was 77 years (range: 28 - 95) with 78 males (62%) and 48 females (38%). Table-1 presents clinical characteristics of the patients. Three clinical subgroups were identified - major bleeding in 61 patients (49%), emergency surgery in 54 patients (43%) and supra-therapeutic INR with high risk of bleeding in 10 patients (8%). Table-2 compares the clinical, laboratory, management and outcome characteristics in these subgroups. According to clinicians' preference, 56% of patients received PTx-VF alone, while 44% received PTx-VF + FFP. Statistically there were no differences in median INR values performed within 6 - 12 hours after administration of PTx-VF vs PTx-VF + FFP in all patients (P = 0.10), bleeding subgroup (P = 0.08) and emergency surgery subgroup (P = 0.24); and the number of patients in the supra-therapeutic INR subgroup was very small for evaluation. Overall 4 patients died due to warfarin-related complications, all of them in the bleeding subgroup.
Conclusion
In our study majority (64%) of patients were above 75 years and the most common (69%) reason for warfarin anticoagulation was atrial fibrillation, which were similar in other studies. We observed that GI bleeding was the most common cause for warfarin reversal. Rapid INR correction with good clinical haemostasis occurred in most of the patients after administration of PTx-VF +/- FFP. The mortality rate in our cohort was 3% (4 of 125), and intracranial bleeding accounted for 75% (3 of 4) deaths. Among 14 patients who experienced intracranial bleeding, either spontaneous or induced by trauma, three (21%) died. There were no significant differences in the post-treatment INR values with PTx-VF alone when compared to PTx-VF + FFP, overall and also in the clinical subgroups. The major advantage of warfarin over DOACs is the rapid reversibility in emergency settings and we demonstrated that our 3-factor PCC (PTx-VF) was effective in emergency reversal of warfarin, without the need for FFP. There are a few limitations in this study since it is retrospective and observational. Hence prospective studies are required for better evaluation of the clinical characteristics, and the efficacy of 3-factor PCC without FFP in emergency reversal of warfarin anticoagulation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.